PLANO PAIN TREATMENTS
LEARN HOW WE CAN HELP
Home » Treatments
CENTERS & INSTITUTES
Interventional Pain Treatments
Read about some of the pain treatments we offer at The Pain Relief Center!
- Adhesiolysis
- Alternative Medicine
- Ankle Injections
- Back Pain Treatments
- Botox Migraine Treatment
- Botox Therapy for Neuromuscular Disorders
- Caudal Steroid Injection
- Carpal Tunnel Treatment
- Celiac Plexus Block
- Cervical Steroid Injection
- Combination Analgesics
- Continuous Catheter Nerve Blocks
- Disc Denervation
- Ergotamines
- Epidural Steroid Injection
- ESTIM
- Facet Injections
- Ganglion Impar Block
- Hip Injections
- Hormone Replacement Therapy
- Intercostal Nerve Block
- Interscalene Block
- Joint Injections
- Knee Gel Injections
- Lumbar Epidural Steroid Injection
- Lumbar Sympathetic Block
- Lumbar Transforaminal Epidural Steroid Injection
- Medial Branch Blocks
- Medication Management for Chronic Pain
- Natural Treatments
- Occipital Nerve Block
- Occipital Nerve Stimulation
- Percutaneous Discectomy
- Peripheral Nerve Stimulation
- Radiofrequency Ablation
- Rhizotomy (RF)
- Sacroiliac Joint Injections
- Sphenopalatine Ganglion Block
- Spinal Cord Stimulator
- Spinal Cord Stimulator Implants
- Stellate Ganglion Block
- Superior Hypogastric Plexus Block
- Sympathetic Nerve Block
- Therapy
- Trigger Point Injections
- Triptans
Custom Pain Relief Treatments and Procedures
The Pain Relief Center provides a plethora of unique, custom pain relief treatments and procedures all with one specific objective: to give each patient the ultimate experience in same-day procedures, an unrivaled quality of care in a state-of-the-art Dallas-Fort Worth and Plano area facility, as well as a highly trained and specialized staff.
Whether you suffer from arthritis, neuropathy, reflex sympathetic dystrophy, complex regional pain syndrome, chronic back pain, neck pain or other conditions that affect your quality of life, The Pain Relief Center can provide the treatment and pain management you seek.

Noninvasive Procedure
Pain Management Doctor, Dr. Rodriguez, offers the best and most advanced noninvasive procedures and benefits. Your body has already experienced trauma and the very treatment you receive for your life-altering pain should not inflict more. Available noninvasive treatments include Trigger Point Injections to ease chronic muscle knots and spasms, as well as Rhizotomy to block pain signals from nerves pinched by a degenerative facet joint.
Patients for whom typical chronic pain treatment regimens have been ineffective in mitigating excruciating back pain can find relief with Spinal Cord Stimulation. A small electric pulse from a discrete device implanted below the skin interrupts the pain signals traveling to the brain and offers reprieve of reflex sympathetic dystrophy, complex regional pain and the effects of failed back surgeries.
Targeted & Precise Treatments
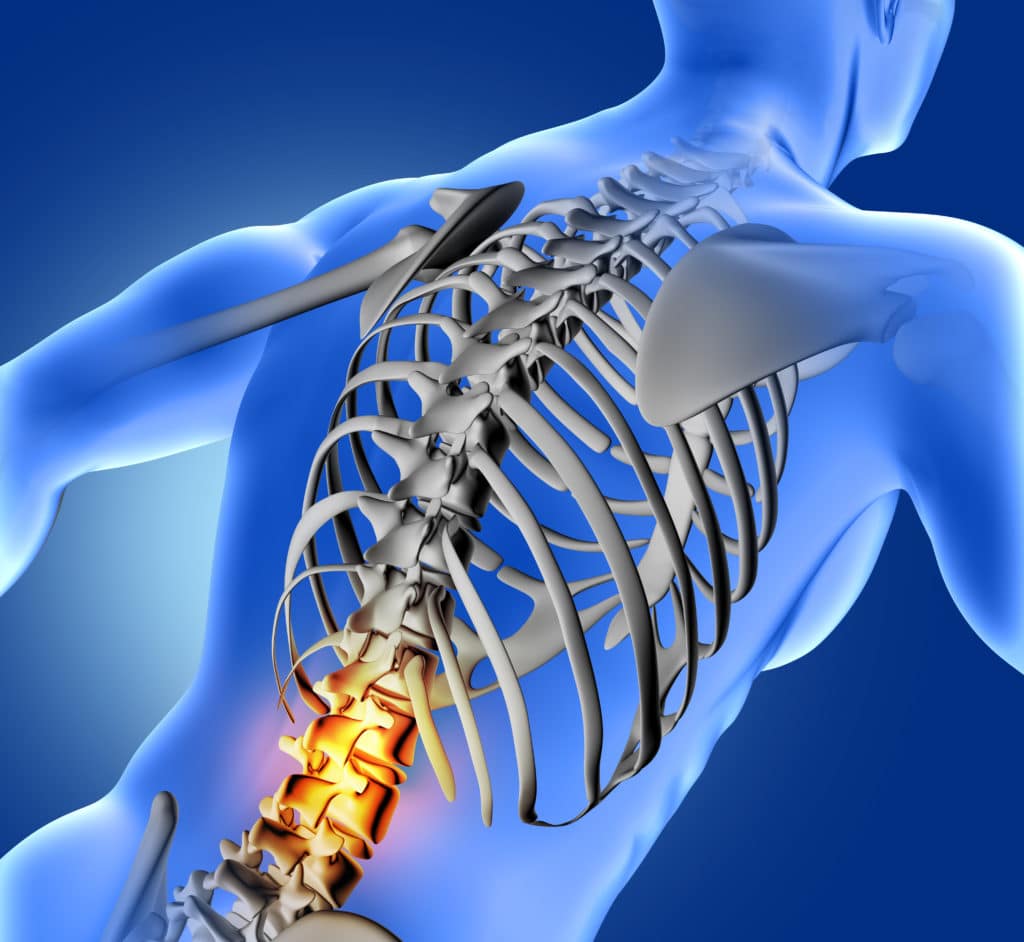
Using state-of-the-art tools and procedures, The Pain Relief Center conducts the groundbreaking process of Pain Mapping, which allows for the precise pinpointing and isolation of specific nerve groups affected.
Dr. Rodriguez uses real-time, medication-filled X-ray injections to isolate treatment to the local source of your chronic pain in a rare but highly effective technique to deliver such treatments as a Lumbar Sympathetic Block and Cervical Epidural Steroid Injections.

Holistic Treatments
Your severe and chronic pain is not a cut that requires only a band-aid. It is a complex, constant physical and emotional experience. For this reason, pain relief physician Dr. Rodriguez focuses on non opioid treatments and medications. While opioid treatments have proven effective in conservative applications, prolonged use or higher doses are shown in research to be ineffective and potentially harmful.
The Pain Relief Center offers a range of holistic treatments to augment clinical procedures and medications. Our highly trained staff provides instruction on the use of compound creams, stretching regimens and yoga, among others. Your pain is multifaceted and your Pain Relief treatment should be as well.
TAKE ACTION
The most critical step on the path to recovery is finding a pain management doctor who can address your pain management needs successfully. The Pain Relief Center and its five specialized institutes are dedicated to meeting any and all of a patient’s needs. Located in the Dallas-Fort Worth area, Dr. Rodriguez and his friendly staff will help you along the path to recovery.
Our new center in Dallas is part of a nationwide development by Pain Relief Centers, geared to providing individualized and comprehensive healing and pain management services with unprecedented levels of compassion, care, and comfort for each patient.