SPINAL STENOSIS
Home » Conditions » Spinal Stenosis
CENTERS & INSTITUTES
Stenosis, in the medical sense, indicates the abnormal narrowing of any particular body channel. Spinal Stenosis is, therefore, the narrowing of the bone channel occupied by the spinal nerves and the spinal cord.
The Neck Structure Includes:
- 7 Vertebrae
- Inter-vertebral Discs
- Joints
- Spinal Cord
- 8 Nerve Roots
- Vascular Elements
- 32 Muscles
- Ligaments
The Neck Is Capable Of Moving Your Head In Many Directions:
- 7 Vertebrae
- Inter-vertebral Discs
- Joints
- Spinal Cord
- 8 Nerve Roots
- Vascular Elements
- 32 Muscles
- Ligaments
Spinal Anatomy
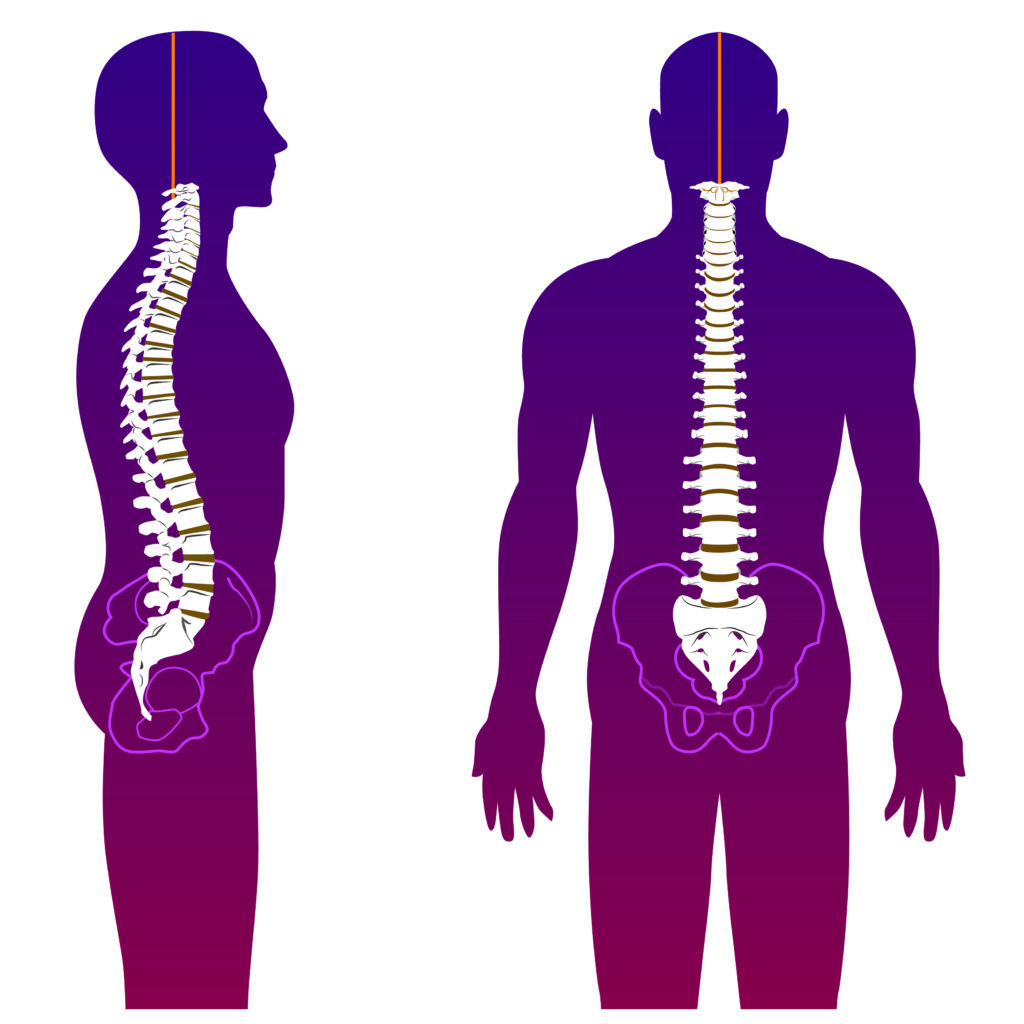
To understand how stenosis affects the spine, it is helpful to know something about spinal anatomy.
First of all, the spinal cord, through which nerves pass from the brain to the rest of the body, is protected by the vertebral column. Imagine the vertebral column as stacks of blocks, called vertebrae, running from the sacrum up to the neck and skull. Each vertebra has bony attachments that stabilize the spine and add another layer of protection to the spinal cord.
Within the vertebral column, there is a large central canal through which the spinal cord passes. On each side of the canal, there are tiny holes called neuroforamen that allow spinal nerves to escape. In a spine that is not affected by spinal stenosis, there is ample room for the spinal cord and spinal nerves, within the central canal. However, in a spine affected with spinal stenosis, bony growths in the spine narrow the central canal, constricting the spinal cord and spinal nerves.
What Causes Spinal Stenosis?
Spinal stenosis is unfortunately usually just a symptom of age, especially lumbar stenosis. However, lumbar stenosis can sometimes develop in younger people who suffer a spinal injury, or who have a congenital curvature of the spine. Deterioration of the facet joints in the back of the spine can also contribute to spinal stenosis.
With cervical stenosis, the narrowing of the central canal is also often just a symptom of age, but it can be exacerbated by conditions like osteoarthritis.
Anything that narrows the spinal canal can contribute to spinal stenosis: herniated discs, bone spurs, or swollen ligaments can all be contributing factors.
What Are The Symptoms Of Spinal Stenosis?
There are two types of spinal stenosis: lumbar, and cervical. Lumbar stenosis occurs in the lower back, while cervical stenosis occurs in the neck. There are some symptoms, however, that are common to both types of stenosis, such as:
- Pain that comes and goes, rather than pain that is continuous
- Pain that occurs with certain activities or positions
- Feeling relieved by resting positions like sitting or lying down
These symptoms usually develop slowly over time.
There are some symptoms that are unique to the two types of spinal stenosis. For instance, people who suffer from lumbar stenosis will typically notice symptoms like:
- Tingling, weakness, or numbness in the lower back and legs
- Leg pain when walking
Those who suffer from cervical stenosis may see similar symptoms but centered closer to the neck. It can lead to symptoms such as extreme weakness or even paralysis.
How is Spinal Stenosis Diagnosed?
- CT
- Selective Nerve Root Block
- MRI
Most of the time when diagnosing spinal stenosis, doctors will order an MRI or a CT scan, or sometimes both. CT scans can reveal abnormal growth in the bone, like bone spurs, which may cause spinal stenosis, while MRIs are designed to reveal soft tissue damage. MRIs can reveal the soft tissue causes of spinal stenosis such as disc bulges and disc herniations.
Some forms of cervical spinal stenosis can be also be diagnosed with a selective nerve root block. In this procedure, a small dose of local anesthetic will be injected into the nerve that is suspected to be compressed by the narrowing spinal canal. If the patient experiences relief, the diagnosis of cervical stenosis is confirmed.
How is Spinal Stenosis Treated?
There are surgical and nonsurgical treatments available to help heal spinal stenosis. Surgical treatments will usually only be necessary is nonsurgical treatments do not provide any relief.
Nonsurgical
Some of the more common nonoperative treatments include:
Exercises
Nearly every treatment program for spinal stenosis will include an exercise and physical therapy regimen. While this will not cure spinal stenosis, it is important that those who suffer from spinal stenosis remain as active as they can, to avoid becoming further debilitated by inactivity.
A short stint with a physical therapist is all most people need to transition to their own exercise program at home.
Some effective exercises that patients find helpful, especially patients suffering from lumbar stenosis, are:
- Riding a bicycle. Depending on the severity of the stenosis, stationery biking may be preferable
- Swimming, or water therapy
- Tai Chi, a type of exercise which involves slow, deliberate, and flowing movements
Higher impact exercises like jogging and contact sports like football and soccer should be avoided.
Activity Modification
People with spinal stenosis are typically advised to avoid any activities that aggravate their symptoms. This will usually include physical activities like running or any contact sports.
Some activities may simply need to be adjusted; for example, many people with spinal stenosis report that leaning forward eases their symptoms. Patients might be advised to bicycle while leaning forward over their handlebars or to lean on a walker or on a shopping cart while walking for long periods of time. It can also provide relief to sit in a recliner instead of in a hardback chair.
Epidural Injections
Occasionally, an injection of cortisone into the epidural space can relieve the symptoms of spinal stenosis. There are concerns about the repeated use of epidural injections and how it affects patients who are at risk for osteoporosis-related fractures, and about the overall efficacy of them, but it is still a common treatment offered by a large number of physicians.
Medications
Anti-inflammatory medications such as aspirin or ibuprofen can be helpful in relieving some of the pain associated with spinal stenosis. Carefully monitored usage of narcotic medication can help with the most severe instances of nerve pain. Anti-depressants are also occasionally prescribed, as well as muscle relaxers and nerve desensitizing medications.
Surgery
There are multiple techniques used to surgically correct spinal stenosis, though there are certain elements that are common to all approaches. The goal of spinal stenosis surgeries is to relieve pressure on the nerves, and the outcome of these surgeries is usually very positive.
Laminectomy
This is the most preferred method for surgically treating spinal stenosis. The area of bony compression will simply be removed. In recent years, the incisions required to do this have become smaller and smaller with the advancement of surgical technology. In some cases, a fusion of the vertebrae may be necessary along with the laminectomy procedure, so that the vertebral column will be stable.
Anterior Cervical Discectomy and Fusion
With this procedure, a damaged disc is removed in order to relieve the pressure on the spinal cord or nerve roots associated with spinal stenosis. A bone graft or implants will be placed where the disc originally was to provide stability and strength to the area.
Interspinous Process Devices
This procedure has been successful for some central canal stenosis patients, but not all patients have benefited from it. Titanium surgical hardware will be inserted into the spinal area and widen out the neuroforamen, allowing more room for the nerve roots to pass out of the spinal column and into the legs.
Facet Replacement or Total Element Replacement
This procedure is somewhat experimental, and research into some of these devices has even been discontinued. It involves either a partial or complete replacement of the facet joints in the back of the spine in order to maintain spinal movement. These facet joints will be replaced by different types of hardware, depending on the severity of the spinal stenosis, as well as its location.
More Conditions
- Achilles Tendinitis
- Allergies
- Arthritis
- Back Pain & Low Back Pain
- Bulging Disc
- Car Accident Injuries
- Carpal Tunnel Syndrome
- Cervicogenic Headache
- Chronic Pain
- Cluster Headache
- Degenerative Disc Disease
- Fibromyalgia
- Foot Pain
- Interstitial Cystitis
- Joint Pain
- Knee Pain
- Low Estrogen
- Neck Pain
- Occipital Neuralgia
- Osteoarthritis
- Osteoporosis
- Piriformis Syndrome
- Plantar Fasciitis
- Reflex Sympathetic Dystrophy (RSD)
- Rheumatoid Arthritis
- Rotator Cuff Tear
- Sacroiliitis Pain
- Sciatica
- Scoliosis
- Shingles
- Shoulder Pain
- Spinal Pain
- Spinal Stenosis
- Tension Headache
- Thoracic Pain
- TMJ
- Trigeminal Neuralgia
TAKE ACTION
The most critical step on the path to recovery is finding a pain management doctor who can address your pain management needs successfully. The Pain Relief Center and its five specialized institutes are dedicated to meeting any and all of a patient’s needs. Located in the Dallas-Fort Worth area, Dr. Rodriguez and his friendly staff will help you along the path to recovery.
Our new center in Dallas is part of a nationwide development by Pain Relief Centers, geared to providing individualized and comprehensive healing and pain management services with unprecedented levels of compassion, care, and comfort for each patient.